Bitot's spots in vitamin A deficiency
The patient is a 49-year-old male that presented to the emergency department with complaints of bilaterally decreased vision, particularly in dim illumination, and eye pain.
His previous medical history was remarkable for hemodialysis due to renal vascular disease and chronic hepatitis due to severe alcoholism; there was also a history of long-standing poor visual acuity in the OD due to a central retinal vein occlusion (CRVO) many years ago.
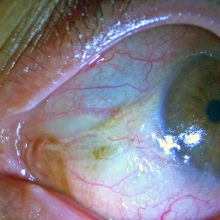
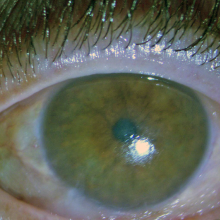
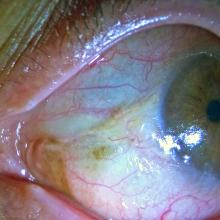
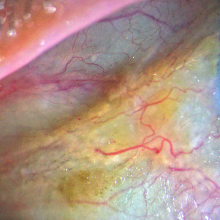
Visual acuities were hand motion in the OD and finger counting in the OS. Biomicroscopy revealed extreme bilateral corneo-conjunctival xerosis, scaly patch foamy lesions on the paralimbal temporal and nasal areas of both eyes. In the OD, two corneal ulcers with infiltrates, mixed hyperemia and an inflammatory mass in the anterior chamber were also found. Fundoscopy was normal in the OS and impossible due to media opacity in the OD. OD ocular ultrasonography was negative for vitritis.
The diagnosis was confirmed (retrospectively, after discharge) by evidence of low serum retinol levels (0.2 µM; reference adult range 0.7-2.8 µM).
Vitamin A deficiency, with pathognomic Bitot's spots.
A medical history notable for a high risk of malnourishment and altered hepatic metabolism, complaints of decreased vision and nyctalopia, corneo-conjunctival xerosis and the presence of lesions compatible with Bitot’s spots lead to a preemptive diagnosis of xerophthalmia due to vitamin A deficiency.
He was admitted for therapy with fortified topical antibiotics (ceftazidime 50 mg/ml and vancomycin 33 mg/ml) in the OD and an intense regimen of preservative-free ocular lubricants bilaterally. While awaiting for the determination of serum retinol levels, empirical supplementation was initiated with oral retinol (200.000 IU on day 1, followed by the same dosage on day 2 and day 7 and 8 of admission) as per the WHO protocol, accompanied by topical therapy with a retinoic acid ointment 50.000 IU/g twice daily.
At discharge (day 10) the patient referred resolution of nyctalopia and a marked increase in visual acuity, particularly in the OS which improved to 20/40 without correction and to a best corrected visual acuity of 20/25. Despite a significant bilateral improvement in the ocular surface with resolution of the xerosis, the Bitot’s spots persisted.
Bitot’s spots are considered pathognomic of vitamin A deficiency and correspond to triangular patches of squamous keratinous metaplasia of the conjunctival epithelium, usually near the limbus, typically at the three o’clock and/or nine o’clock positions. The foamy aspect is attributable to colonization by gas-producing bacteria (p.e. Corynebacterium xerosis). Although vitamin A deficiency is relatively uncommon in developed nations, it can be found in malnourished patients with other comorbidities that promote an altered metabolism, as in this case. Extreme conjunctival xerosis in such context, even in the absence of Bitot’s spots, should lead to a low threshold for empirical supplementation and vitamin A level testing.
Duignan E, Kenna P, Watson R, Fitzsimon S, Brosnahan D. Ophthalmic manifestations of vitamin A and D deficiency in two autistic teenagers: case reports and a review of the literature. Case Rep Ophthalmol. 2015;6(1):24-9.
Ferrari G, Viganó M. Images in clinical medicine. Bitot's spot in vitamin A deficiency. N Engl J Med. 2013;368(22):e29.
Mclaren DS. Bitot's spots: a review of their significance after 100 years. Br Med J. 1963;2(5362):926.
Mclaughlin S, Welch J, Macdonald E, Mantry S, Ramaesh K. Xerophthalmia--a potential epidemic on our doorstep?. Eye. 2014;28(5):621-3.
Sharma A, Aggarwal S, Sharma V. Bitot's Spots: Look at the Gut. Int J Prev Med. 2014;5(8):1058-9.